April 4, 2025
The Anatomy of a Ligament
Before understanding the details of a tear, it’s essential to understand the fundamental structure of a ligament. Ligaments are primarily composed of collagen fibers, arranged in a dense, parallel pattern, providing exceptional tensile strength. This arrangement allows them to withstand significant forces while maintaining flexibility. They are also richly supplied with nerves, containing nerve endings that provide feedback to the brain about joint position and movement.
Causes of Ligament Tears
Ligament tears typically occur due to sudden, forceful movements that exceed the ligament’s capacity. Common causes include:
- Sports Injuries:Twisting, pivoting, sudden changes in direction.
- Falls and Accidents:Abnormal joint forces.
- Overuse and Repetitive Strain: chronic overuse can weaken ligaments over time, making them more susceptible to tears.
- Direct Blows:A direct impact to a joint can cause significant ligament trauma.
- Sudden Twisting or Bending:Exceeding normal range of motion.
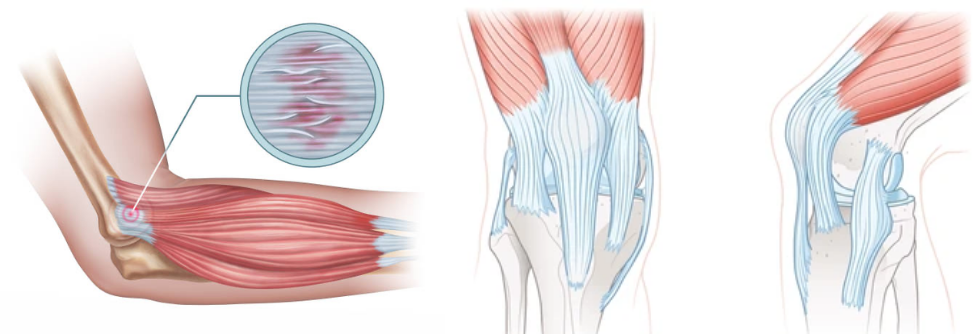
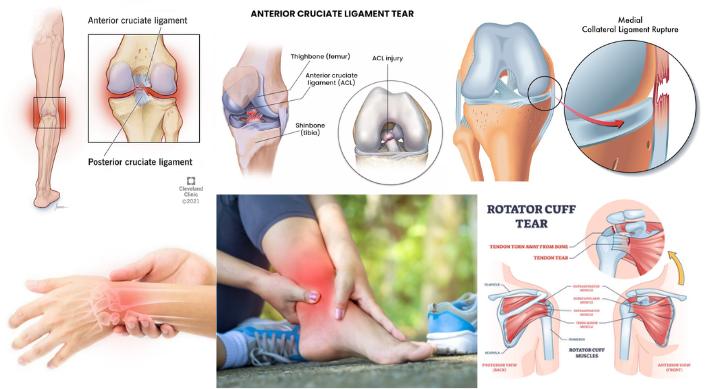
Common Locations and Types of Ligament Tears
Ligament tears can occur in various joints throughout the body, but some are more common than others:
Source: Cleveland Clinic
- Ankle Ligament Tears (Sprains):The lateral ankle ligaments, particularly the anterior talofibular ligament (ATFL), are frequently injured in ankle sprains.
- Knee Ligament Tears:
- Anterior Cruciate Ligament (ACL) Tears:Often occurring during pivoting or landing from a jump, ACL tears are common in athletes.
- Medial Collateral Ligament (MCL) Tears:Usually caused by a direct blow to the outside of the knee.
- Posterior Cruciate Ligament (PCL) Tears:Typically result from a direct impact to the front of the knee, such as a dashboard injury.
- Lateral Collateral Ligament (LCL) Tears:Less common, usually caused by a blow to the inside of the knee.
- Wrist Ligament Tears:The scapholunate ligament, connecting the scaphoid and lunate bones, is prone to tears from falls onto an outstretched hand.
- Shoulder Ligament Tears:The ligaments supporting the shoulder joint, particularly the glenohumeral ligaments, can be injured during dislocations or forceful movements.
Degrees of Ligament Tears
Ligament tears are classified into three grades, based on the severity of the injury:
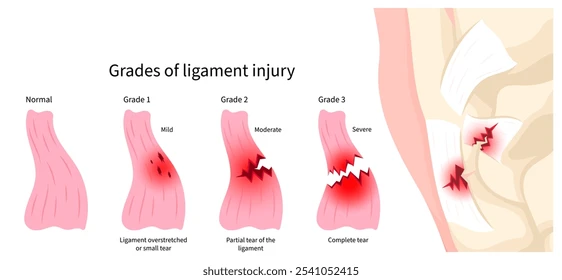
- Grade 1 (Mild):The ligament is stretched or slightly torn, but joint stability is maintained. Symptoms include mild pain, swelling, and tenderness.
- Grade 2 (Moderate):The ligament is partially torn, resulting in some joint instability. Symptoms include moderate pain, swelling, bruising, and difficulty bearing weight.
- Grade 3 (Severe):The ligament is completely ruptured, leading to significant joint instability. Symptoms include severe pain, significant swelling, bruising, and inability to bear weight. A “popping” sensation may be felt or heard at the time of injury.
Symptoms of Ligament Tears
The symptoms of a ligament tear can vary depending on the severity of the injury and the affected joint. Common symptoms include:
- Pain: ranging from mild to severe, depending on the grade of the tear.
- Swelling:Swelling occurs as a result of inflammation and fluid accumulation in the injured area.
- Bruising:may appear as blood vessels rupture due to the injury.
- Instability:A feeling of looseness or giving way in the joint.
- Limited Range of Motion:Difficulty moving the joint through its normal range of motion.
- Popping or Tearing Sensation:can be felt at the time of injury.
- Tenderness:The injured area may be tender to the touch.
Diagnosis of Ligament Tears
Diagnosing a ligament tear involves a thorough physical examination and imaging studies.
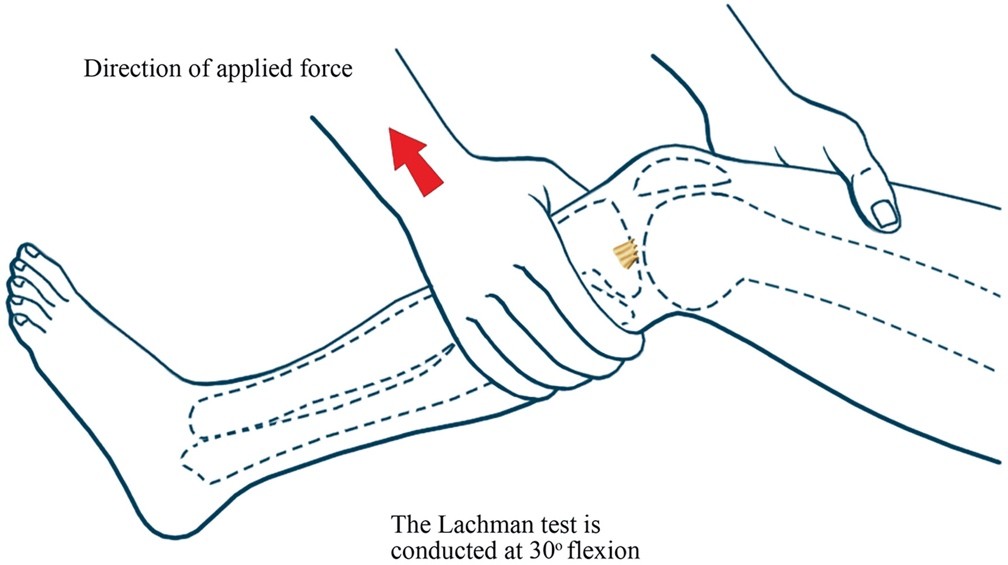
- Physical Examination:A healthcare professional will assess the joint’s stability, range of motion, and tenderness. Specific tests, such as the Lachman test for ACL tears or the anterior drawer test for ankle sprains, may be performed.
Source: Sage Journals
- Imaging Studies:
- X-rays: X-rays are used to rule out fractures or other bone injuries.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of soft tissues, allowing for accurate diagnosis of ligament tears and assessment of their severity.
- Ultrasound: Ultrasound can be used to visualize ligament injuries, particularly in superficial joints.
Treatment of Ligament Tears
Treatment for ligament tears depends on the severity of the injury, the affected joint, and the individual’s activity level.
- Non-Surgical Treatment (Conservative Management):
- RICE Protocol:Rest, ice, compression, and elevation are essential for managing acute ligament injuries.
- Pain Medication:Over-the-counter or prescription pain relievers can help manage pain and inflammation.
- Physical Therapy:Physical therapy is crucial for restoring joint stability, strength, and range of motion.
- Bracing or Splinting:Braces or splints can provide support and immobilization to the injured joint.
- Surgical Treatment:
- Ligament Reconstruction:Involves replacing the torn ligament with a graft, often taken from another part of the body (autograft) or from a donor (allograft).
- Ligament Repair:In some cases, the torn ligament can be repaired directly.
- Arthroscopy:A minimally invasive surgical technique that uses small incisions and a camera to visualize and repair the injured joint.
Rehabilitation and Recovery
A comprehensive rehabilitation program typically includes:
- Phase 1: Acute Phase (Initial Healing):Focuses on pain and swelling management, gentle range of motion exercises, and protected weight-bearing.
- Phase 2: Subacute Phase (Early Strengthening):Emphasizes restoring joint stability, increasing range of motion, and initiating strengthening exercises.
- Phase 3: Functional Phase (Advanced Strengthening):Progresses to more challenging exercises, including sport-specific training, to prepare for return to activity.
- Phase 4: Return to Activity Phase:Focuses on gradual return to sports or other activities, with continued emphasis on strengthening and stability.
Prevention of Ligament Tears
While some ligament injuries are unavoidable, several measures can help reduce the risk:
- Warm-up and Cool-down:Proper warm-up and cool-down routines prepare muscles and ligaments for activity and reduce the risk of injury.
- Strength Training:Strengthening the muscles surrounding the joints provides added support and stability.
- Flexibility Exercises:Maintaining flexibility helps prevent excessive stress on ligaments.
- Appropriate Equipment:Wearing appropriate protective equipment, such as braces or supports, can help prevent ligament injuries.
- Balance Training:Balance training improves proprioception and coordination, reducing the risk of falls and other injuries.
- Avoid Overuse:Gradually increasing activity levels and avoiding overuse can help prevent chronic ligament injuries.
Conclusion
Ligament tears can be debilitating injuries, but with prompt diagnosis, appropriate treatment, and dedicated rehabilitation, individuals can regain joint function and return to their desired activities. Understanding the anatomy, causes, symptoms, and treatment options for ligament tears is crucial for both prevention and effective management.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Please consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.
References:
- Benjamin, M., & Ralphs, J. R. (1998). Fibrocartilage in tendons and ligaments—an adaptation to compression. Journal of Anatomy, 193(Pt 4), 481–494.
- Beynnon, B. D., Fleming, B. C., Johnson, R. J., Nichols, C. E., & Renström, P. A. (2002). Anterior cruciate ligament strain behavior during rehabilitation exercises in patients treated with patellar tendon grafts. The American Journal of Sports Medicine, 30(1), 27–34.
- Orchard, J., Seward, H., Orchard, S., & Alcott, E. (2002). Results of 2 decades of weather surveillance of Australian Football League injuries. British Journal of Sports Medicine, 36(2), 135–138.
Renström, P. A., Johnson, R. J., & Arms, S. W. (1986). Prevention of knee ligament injuries. Sports Medicine, 3(2), 123–141