February 24, 2025
Ankle Instability: Navigating the Path to Stability
Understanding Ankle Instability
Before exploring management strategies, it’s crucial to understand the underlying mechanisms of ankle instability. The ankle joint is primarily stabilized by three ligaments: the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL). These ligaments, particularly the ATFL, are frequently injured during inversion sprains, a common mechanism of ankle injury.
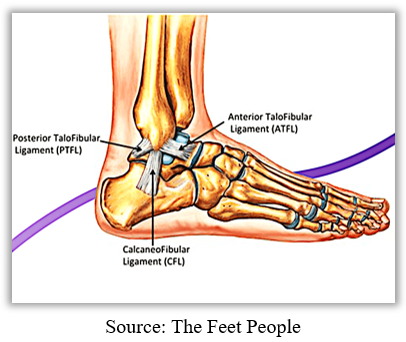
When these ligaments are damaged, the ankle joint becomes less stable, making it more susceptible to further injury. This can lead to a vicious cycle of recurrent sprains, chronic pain, and functional limitations.
Ankle instability is a spectrum of conditions, ranging from mild to severe.
- Mild: Occasional feelings of giving way, minor discomfort.
- Moderate:Frequent episodes of instability, significant pain and functional limitations.
- Severe:Chronic instability, persistent pain, and significant functional disability.
Causes:
- Acute ankle sprains: The most common cause, typically involving inversion injuries (rolling the ankle outwards).
- Chronic ankle instability: Recurrent sprains weaken the ligaments, leading to persistent instability.
- Other factors: Previous ankle fractures, neurological conditions, and certain foot deformities.
Non-Surgical Management
Non-surgical approaches are the first line of treatment for most cases of ankle instability.
Conservative Treatment:
- Rest, Ice, Compression, Elevation (RICE): Immediate management after an acute sprain to reduce inflammation and pain.
- Pain Management: Over-the-counter pain relievers (e.g., ibuprofen, acetaminophen) can help alleviate discomfort.
- Bracing and Taping: Provides support and stability to the ankle joint, reducing the risk of further sprains.

Physical Therapy:
- Strengthening Exercises: Focus on strengthening the muscles around the ankle, including calf muscles, peroneal, and anterior tibialis.
- Balance and Proprioception Training: Improve balance and coordination through exercises on unstable surfaces (e.g., balance boards, foam pads).
- Flexibility Exercises: Maintain and improve ankle range of motion.
Functional Training:
- Sport-Specific Exercises: Incorporate exercises that mimic the demands of the individual’s sport or activity.
- Gradual Return to Activity: A progressive approach to returning to full activity levels, minimizing the risk of reinjury.
Footwear Modifications:
- Supportive Footwear: Choosing shoes with adequate support and cushioning can help reduce stress on the ankle.
- Custom Orthotics: In some cases, custom orthotics can provide additional support and improve foot biomechanics.
Surgical Management
Surgical intervention is considered when non-surgical approaches fail to provide adequate relief or in cases of severe instability.
- Ligament Reconstruction:
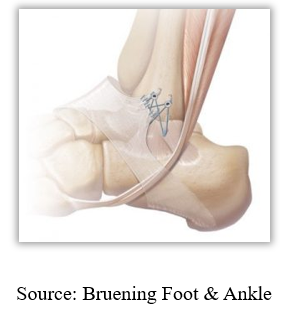
- Broström Procedure: The most common procedure, involving tightening or reconstruction of the damaged lateral ligaments.
- Other Techniques: Various techniques may be used depending on the specific injury and patient factors.
Tendon Transfers:
In some cases, tendons from other areas of the body may be transferred to reinforce the weakened ligaments.
Arthroscopic Surgery:
Minimally invasive procedures can be used to assess the extent of damage and perform ligament repairs.
Rehabilitation After Surgery
Post-operative rehabilitation is crucial for optimal recovery and return to function.
- Early Mobilization: Gentle range-of-motion exercises are initiated soon after surgery.
- Progressive Strengthening: Gradually increase the intensity and complexity of strengthening exercises.
- Balance and Proprioception Training: Continue to improve balance and coordination.
- Return to Activity: A gradual and supervised return to sports and other activities is essential.
Prevention of Ankle Instability
- Proper Footwear: Wear appropriate footwear for the activity.
- Strength and Conditioning: Maintain good muscle strength and flexibility around the ankle.
- Warm-up and Cool-down: Proper warm-up and cool-down routines can help prevent injuries.
- Proper Technique: Maintain good technique during sports and other activities.
- Address Underlying Conditions: Treat any underlying conditions that may contribute to ankle instability.
Conclusion
Ankle instability can significantly impact an individual’s quality of life. A multidisciplinary approach, including conservative management, physical therapy, and in some cases, surgery, is often necessary for optimal outcomes. Early intervention and adherence to the recommended treatment plan are crucial for restoring stability, reducing pain, and improving function. By working closely with healthcare professionals, individuals with ankle instability can effectively manage their condition and return to their desired level of activity.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Please consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.
References:
- American Academy of Orthopaedic Surgeons. (n.d.). Ankle Instability. Retrieved from https://orthoinfo.aaos.org/en/recovery/foot-and-ankle-conditioning-program/
- National Institutes of Health. (n.d.). Ankle Sprains. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279552/
- The American Journal of Sports Medicine. (2010). Ankle Sprains – Recommendations for Treatment and Rehabilitation. Retrieved from https://www.primarycaresportsmedicine.com/wp-content/uploads/2016/12/ANKLE-ANKLE-ATF-SPRAIN.pdf